Clinical practice influences the development of Clinical Practice Guidelines (CPGs)
CPG development, through PHECC’s Medical Advisory Group (MAG) is influenced by many factors, not least national and international clinical practice.
Recently, Michael Donnellan, an Advance Paramedic (AP), identified a clinical issue that causes patient distress during long journeys to hospital – motion sickness.
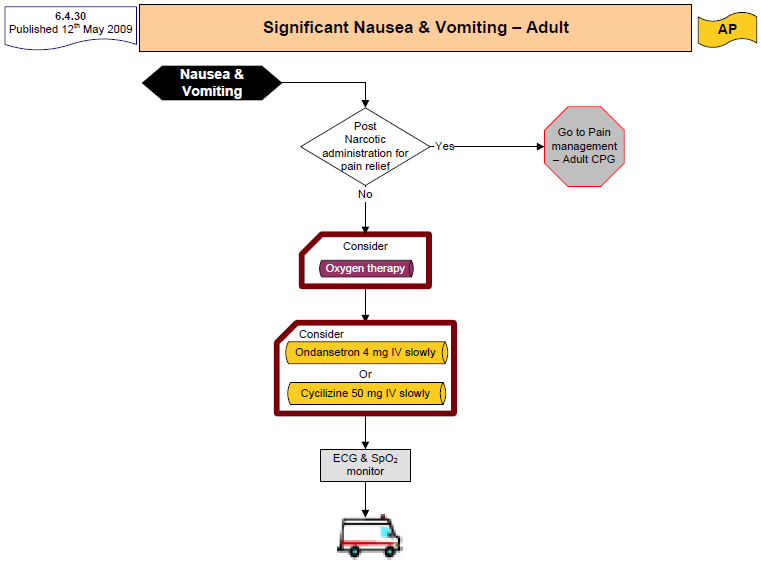
Michael presented a case study and suggested that existing medications in the medication formulary could have their indications expanded to include nausea and vomiting other than that following Morphine administration.
The case study was presented to MAG and following a review of pre-hospital clinical practice literature it was agreed that it would be safe and effective to introduce a new CPG to incorporate this condition.
The new CPG, Significant Nausea & Vomiting – Adult was agreed and will be included in the 3rd Edition CPGs, due out this summer
Case Study: Antiemetic used in pre hospital environment
|
Background
Ambulance crew: Michael Donnellan, AP and Cathal McDonnell, P.
Transport Distance
68 miles from patient’s residence to UCHG.
Ambulance was called to the home of a 79-year-old male, who had fallen and sustained injuries to his left shoulder. His GP had seen him and requested ambulance transport to UCHG Galway.
History of presenting complaint
Patient had fallen the previous day, had become very uncomfortably due to pain and was unable to sleep. Patient was a non-insulin dependent diabetic.(Glucophage) MI in 2003 (Stent). Patientrefused all form of analgesia. Pain 5/10, also refused IV access.
Problems experienced on transport
After several miles of transport the patient complained of nausea. Measures were taken to make the patient more comfortable, i.e. reduced ambulance speed, opened windows for more ventilation, reduced heat in the back of ambulance, all to no avail. The patient became very uncomfortable and started to become increasingly agitated because of his severe vomiting. |
|
Actions taken
The AP called the patient’s GP who was on duty, and informed her of the patient’s condition. GP requested that the patient be brought to her surgery which was en route to the hospital. She also gave instruction that the AP gain IV access. The GP administered 12.5 mg of Stemitil to the patient. After several minutes the patient’s condition improved, and all vomiting and feeling of nausea subsided. During the remainder of the journey the patient was content and comfortable and had no further episodes of emesis.
Conclusion
This scenario is frequently encountered by ambulance crews when transporting patients. In this particular case the GP was available to assist. This, however, is not always the case. Due to long transport times and mileage, sometimes in excess of 70 miles, patients often arrive in UCHG in worse condition due to travel sickness. This scenario is very common within the ambulance service and many patients, particularly in more remote areas, have difficulty travelling in the ambulance due to the bad road conditions and poor infrastructure.
The principle of an antiemetic is already in use in the CPGs and a new CPG to include the above situation would assist with improving pre-hospital emergency care practice.
|