Protocol 37-The (time-critical) Emergency Inter-Hospital Transfer Policy
100% of Irish hospitals now accessing Protocol 37
Protocol 37 implementation is now completed, with 46 hospitals listed with access to the emergency inter-hospital transfer service provided by the National Ambulance Service. The number of transfers has been steadily increasing month-on-month as more hospitals have gained access post training.
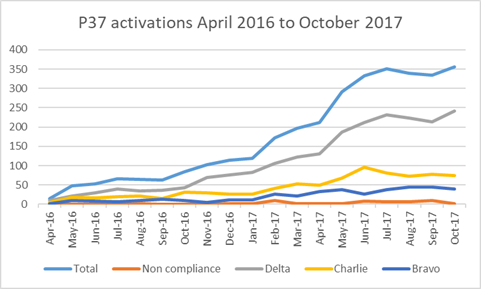
A senior clinician decides that a clinically time-critical inter-hospital transfer is required and contacts the National Emergency Operations Centre Call-taker via 999 / 112. Protocol 37 is activated utilising one of three agreed response times; immediate (Delta), within 30 minutes (Charlie) or within 60 minutes (Bravo).
Protocol 37 implementation was facilitated by a designated Project Lead funded initially by the HSE Clinical Strategy and Programmes Division (CSPD) and the Pre-Hospital Emergency Care Council (PHECC), and for the last year by PHECC alone. This role concludes in December 2017 and to ensure the continued successful implementation of the Protocol 37 service there is a requirement to establish an operational support structure. Arrangements for national oversight, transparent audit with follow-up capability and clear local governance structures are required. The HSE, which is the key stakeholder, is strongly recommended to support the operational implementation of Protocol 37 with the conclusion of PHECC's involvement. Protocol 37 has been developed and successfully rolled out nationally. The operational stage now commences.
Until conclusion of the Project Lead role in December 2017, weekly reports of all Protocol 37 transfers have been provided by HSE/NAS Informatics to the Project Lead. 100% calls have been assessed for compliance with response time and turnaround time in transferring and receiving hospitals, in addition to investigating concerns raised by front line crew regarding appropriateness of the call. The Project Lead has been liaising with a locally designated person(s) in each hospital with responsibility for investigation and communication on any issues arising from transfers in or out of their hospital.
Benefits of the implementation of Protocol 37 are obvious. A survey of hospital clinical staff revealed 100% feel that P37 is useful to them. Access to ambulance crews for time-critical transfers has been simplified by the ‘immediate procurement of an ambulance’, which results in ‘less delays in transferring acutely unwell patients’ and ‘reduces on site complications’ in hospitals without the facility for definitive care for that patient. The streamlined communication process has reduced ‘the amount of time that we spend on the phone arranging the transfer’ and ‘allows for a change in patients’ condition and opportunity to reschedule the transfer’.
However, as with the introduction of any change, the process has not been without its challenges. Frustrations have been expressed around ‘misunderstanding of the use/criteria’ or ‘confusion at ward level over what constitutes’ a Protocol 37 call with the sense that ‘some hospitals do not use the protocol for the right category of patient’.
Although ‘ensuring that it is not abused’ is essential to the success of the Protocol 37 initiative, there is clear division on the burden of the follow-up processes; ‘the audit is invaluable as it flags abuse and allows a targeted enquiry’ versus ‘unexpected delays outside of our control e.g. patient deterioration or doctor delaying transfer & then having to explain this later. Feels like a blame culture’. The named hospital liaison person is obliged to provide ‘feedback on the service when I haven't been there for the event’ and may experience an impact on their daily workload as ‘the reports required…are time consuming’.
Pre-hospital staff are also currently undertaking the same survey. Early responses are mixed. Although there is some support for the protocol when correctly activated, 50% of pre-hospital respondents have stated that Protocol 37 is not useful to them and has placed a considerable, clinically unnecessary burden on pre-hospital resources. This dissatisfaction must be considered, acknowledged and addressed by the future oversight body for Protocol 37. Results will be published in the final P37 Implementation Report.
Of note, inappropriate activations of P37 have been running at <2% for the duration of the project. Unfortunately, these are the calls that receive the most press and cause both a burden on the emergency ambulance service’s ability to respond to community 999 calls and can impact the trust relationship among pre- and in-hospital providers which is critical to maintaining this vital service. Several improvements have been put forward for action to reduce non-compliant activations of P37.
- The online learning and information resources will be hosted open access to facilitate group retraining.
- Some adjustments will be made to the proforma/questioning template in the NEOC for the call-taker including two additional questions:
- Recording of the time-critical diagnosis to reduce inappropriate calls and provide real-time feedback to the ambulance crew
- Recording an additional patient identifier to facilitate hospital response to P37 enquiries.
- Information posters have been developed to highlight the different levels of inter-hospital transfer available to clinicians.
- Hospital group information sessions to be held with hospital liaisons, front line ambulance crew and NEOC staff to share ideas and experiences, build relationships, and develop common understanding and trust.
Continued support and oversight of the Protocol 37 Ambulance Service is essential to ensure improved outcomes for time-critically-ill patients in Irish hospitals. Ongoing monitoring of the service will provide opportunities for shared learning and training for improvement. Collation of national patient outcomes will be invaluable in maintaining this service as a national and international quality benchmark.